Answering Your Questions about Single Cell Applications for SARS-CoV-2 Research
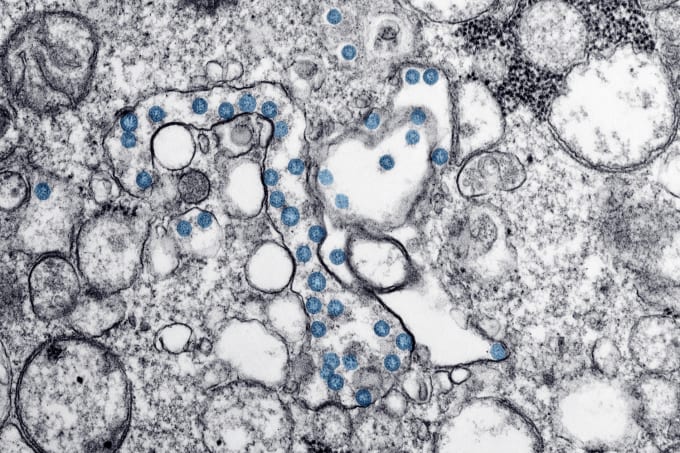
Researchers around the world are responding to the need to understand the underlying biology of the novel coronavirus. They are studying how the virus infects, what determines cell type-specific susceptibility to infection, what degree of immune response distinguishes severe and mild cases, and what antibodies can be leveraged to target and stop the virus.
Though there is much work still to be done, a number of researchers are making great strides, and they’ve incorporated single cell solutions from 10x Genomics into their workflows. In a recent webinar hosted by The Scientist, Brian Fritz, PhD, Associate Director, Strategic Market Development & Programs at 10x Genomics, shared some of the ongoing SARS-CoV-2 research enabled by single cell gene expression and immune repertoire profiling technology. He also discussed the utility of single cell immune profiling in urgent therapeutic interventions for the coronavirus, including its application to accelerate antibody discovery and clarify the clonotypic expansion and transcriptional programs underlying the immune response to vaccination. Watch an on-demand recording of the webinar, and review some of the questions audience members posed to our speaker following his presentation.
Applying single cell sequencing to virology
Can we detect viral RNA in infected cells using single cell RNA-sequencing?
The simple answer is yes. The Chromium Single Cell Gene Expression Solution detects RNA molecules with a poly-A tail. If the viral RNA is polyadenylated and at sufficient concentrations in the tested sample, it should be detected. This was demonstrated in a recent medRxiv pre-print, when a group of researchers from Shenzhen Third People’s Hospital were able to detect viral transcripts from patient samples of bronchoalveolar fluid (BALF) in severe cases of SARS-CoV-2 infection (1). Though further study is required to determine if BALF cells were infected and expressing the virus, or if they were partitioned with viral transcripts due to higher ambient viral load, the use case stands as a powerful demonstration of the ability of single cell sequencing to detect the presence of viral transcripts in severe cases.
A related application of single cell sequencing is to explore how the presence of viral transcripts impacts the transcriptome of infected cells. What host cell signaling pathways are disrupted, what genes are downregulated, what defensive mechanisms are short-circuited as a result of viral infection? These are also critical questions that require further study.
If you’d like to explore more applications of single cell sequencing for virology, take a look at this additional on-demand webinar from 10x Genomics’ Senior Science and Technology Advisor, Hannes Arnold. Watch now →
Single cell analysis accelerates antibody discovery and validation
How can B-cell receptor (BCR) sequencing be used to identify virus-neutralizing antibodies?
This question has been answered directly and beautifully in a recent publication out fromCell: High-Throughput Mapping of B Cell Receptor Sequences to Antigen Specificity. The study, led by Ian Setliff and Andrea Shiakolas from the lab of Ivelin Georgiev at Vanderbilt University, describes a novel method to rapidly map full-length, paired heavy- and light-chain B-cell receptor (BCR) sequences to their corresponding antigens. The team used this method, called LIBRA-seq, to identify a new broadly neutralizing antibody in blood samples from two subjects with HIV.
LIBRA-seq leverages the Chromium Single Cell Immune Profiling Solution with Feature Barcode Technology to tag antigens with a unique oligonucleotide barcode. With this capability, researchers can multiplex a number of different antigens together. This is how it works: researchers can mix antigen reagents with B cells from a patient sample, select for positive binding of antigens via flow cytometric sample prep approaches, and then use this cellular mixture as a substrate for single cell immune profiling analysis. The end result is a sequence-based measurement of both the antigen-specific B-cell clonotype and the corresponding antigen. Though there are other informative approaches available to select antigen-experienced B cells without a barcode, the benefit of LIBRA-seq is its ability to capture this relationship between B-cell receptor and antigen.
LIBRA-seq is now commercialized into our Feature Barcode capabilities. Explore this technology in more detail by watching an on-demand webinar from lead author Ian Setliff.
How many antibodies can we use for CITE-seq?
We haven’t determined a specific upper limit yet. The R&D team at 10x Genomics has been working closely with our Compatible Product Partner BioLegend on large antibody multiplexing datasets, including some that have created multiplex pools of over 200 antibodies. This upper limit will likely be determined by a practical consideration of how many antibodies are actually available with unique and definable specificity. Additionally, this limit could be re-evaluated for individual experiments, depending on how many antibodies are needed to discern all the available cell states that a researcher would like to analyze simultaneously in a single sample.
What are the tools required to generate and test recombinant antibodies starting from data obtained using the V(D)J library solution?
The output of our Single Cell Immune Profiling Solution and Cell Ranger analysis pipeline is paired V(D)J sequence data. This will include the heavy-and light-chain sequence of immunoglobulin variable regions. Using this data, a researcher would then generate synthetic genomic sequence to create a recombinant antibody. They would have to synthesize the V(D)J sequences, clone these into an expression vector, transduce these into cells, culture the cells, and test for the expressed antibody. Then they would have to purify the antibody and perform subsequent validation steps. These steps and associated tools can be found in established literature for synthesis of recombinant antibodies.
Ian Setliff and colleagues at Vanderbilt University conducted a relevant experiment in their application of LIBRA-seq to identify novel antibodies for HIV (2). Once they obtained recombinant antibodies, they tested the binding specificity of these monoclonal candidates to specific HIV epitopes using ELISA. They also tested their monoclonal candidates against a panel of diverse HIV pseudoviruses, to see if the antibody could achieve broad viral neutralization. You can explore their experimental workflow in this research snapshot →
These steps reveal the ultimate significance of antibody discovery efforts. Antibodies must have a specific function: they must bind to a molecular target, which then has a measurable effect. In the case of infectious disease, an antibody will typically bind to viral particles, or to antigens derived from viral particles. By doing so, the antibodies prevent the virus from infecting other cells, handicapping viral proteins required to bind with and enter into host cells. Another outcome of antibody binding to viral particles is targeting these for removal and destruction by other components of the immune response, such as macrophages.
There are other approaches to determine the binding specificity of recombinant antibodies. In the context of a structural biology study, a researcher might co-crystalize the antibody and viral antigen in order to observe the specific chemistry of the binding interactions. Other cell-based assays could yield information about the efficacy of the antibody to prevent viral infection and cell death. ELISA falls somewhere in between these two additional options, leveraging a colorimetric assay to simply determine whether antibodies bind to target antigens or not.
Applying single cell immune profiling to study vaccines
Can this platform help us to predict the safety, efficacy, and potency of vaccines in advance of results from clinical trials?
One way to approach this question is to think about the relevant capabilities of single cell solutions from 10x Genomics. For example, can researchers use single cell immune profiling to assess the T- and B-cell responses from specific sample types to a vaccine or other therapeutic intervention? Yes, they can. Researchers can use this technology to determine if a specific antigen has provoked an immune response, and whether that immune response is shared across the patient population.
However, it would be inappropriate to think that single cell technology by itself could be an arbiter of the safety and efficacy of a vaccine or other therapeutic.
As the global pandemic continues to evolve, we take great hope in the fact that scientists across the world are overcoming research barriers and accelerating their study of infectious disease. And we are proud that solutions from 10x Genomics can support infectious disease researchers in this critical work.
Explore the latest published and pre-print research on SARS-CoV-2 in more detail by watching this on-demand webinar recording: Crucial Applications of Single Cell Gene Expression and Immune Profiling for Infectious Disease Research. Watch now →
To access more webinars, application notes, and pre-prints, visit our COVID-19 and Infectious Disease Resource Page.
References
- M Liao et al., The landscape of lung bronchoalveolar immune cells in COVID-19 revealed by single-cell RNA sequencing. medRxiv. (2020).
- I Setliff et al., High-Throughput Mapping of B Cell Receptor Sequences to Antigen Specificity. Cell. 179, 1636–1646. (2019).
