Distinguishing mild and critical COVID-19 disease severity: from sample prep to insights
Explore the cellular and molecular mechanisms underlying mild and critical COVID-19 with Dr. Diether Lambrechts, who discussed his research during a recent webinar with Nature. Watch the on-demand webinar now to find out more about the innate and adaptive immune response to SARS-CoV-2 and how it drives disease severity.
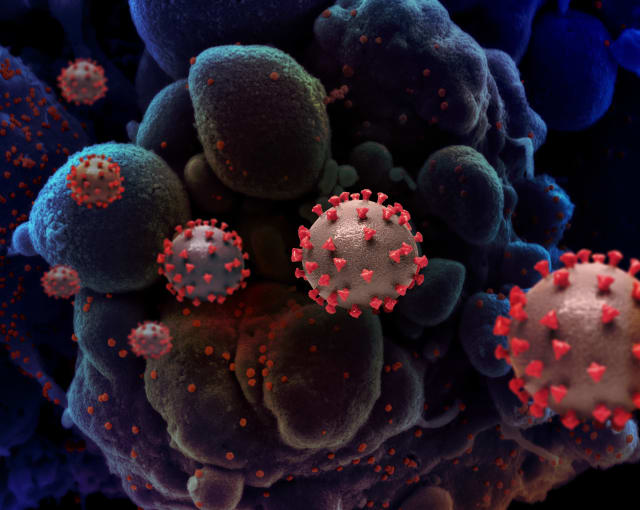
Over the last year, the scientific community has made impressive progress in understanding COVID-19, the disease caused by the SARS-CoV-2 virus, and its underlying biology, but there is still much to discover. We now know that there are three grades of disease severity, each characterized by distinct symptoms, outcomes, and responses to treatment (Siddiqi et al. J Heart Lung Transplant, 2020). However, we don’t know much about the immune mechanisms driving these different levels of severity. Luckily, there are scientists who’ve made it their mission to unravel this mystery.
In a recent webinar hosted by Nature, we heard from Dr. Diether Lambrechts, from the Center for Cancer Biology (CCB), KU Leuven, about his latest research, which focused on the synchronization of innate and adaptive lung immune responses to SARS-CoV-2 during COVID-19. He was particularly interested in the differences in immune and inflammatory responses observed between patients with mild and critical COVID-19 disease severity. Dr. Lambrechts and his colleagues collected bronchoalveolar lavage (BAL) fluid from 22 patients who tested positive for SARS-CoV-2 (classified as either mild or, with the need for respiratory support at the time of sampling, critical) and 13 who displayed pneumonia symptoms but tested negative for SARS-CoV-2. They sought to not only identify the cells driving immune responses, but also to understand how they worked together to determine disease severity.
Using Chromium Single Cell Gene Expression, they characterized the cell types found across samples, comparing the frequencies of those cell types between SARS-CoV-2-positive and SARS-CoV-2-negative patient samples, as well as between SARS-CoV-2-positive mild and critical patient samples. With this method, they were able to track the T-cell and monocyte-to-macrophage trajectories of specific cell types in both mild and critical COVID-19, uncovering mechanisms of inflammatory response in severe cases of the disease.
During the webinar, Dr. Lambrechts discussed the study in detail, describing the methods his team used to make their discoveries while stressing the utility of single cell capabilities in studying the innate and adaptive immune response. He was joined by two of his colleagues for a live Q&A, during which they answered questions on everything from experimental conditions when working with infectious disease samples to cell population identification. Keep reading for a preview of some of the Q&A highlights, then watch the on-demand webinar for yourself, available now.
Processing BSL-3 samples for single cell gene expression
Using the 10x Genomics platform, can we consider the virus to be inactivated in BAL samples after GEM-RT incubation has taken place? When is it safe to transport the samples to a BSL-2 laboratory?
Due to the infectious, respiratory nature of the disease, SARS-CoV-2 experiments require biosafety level 3 (BSL-3) conditions, which means that, immediately following BAL collection, Dr. Lambrechts and his colleagues transported the samples to a BSL-3 laboratory to process them for single cell sequencing. However, Dr. Lambrechts noted that once the reverse transcription reaction, which runs at 65ºC at multiple time points, had taken place, they could then safely transport the samples to a lab at a lower safety level where they continued sample processing and then moved onto sequencing.
To perform scRNA-seq on BAL samples from SARS-CoV-2-positive patients, does the 10x Genomics instrument need to be placed within a BSL-3 facility, or is that level of containment only required for sample preparation?
For SARS-CoV-2 samples, the Chromium instrument does need to be placed in a BSL-3 environment. As mentioned above, it was not safe for the samples to be transported to a lower safety level until after reverse transcription had taken place.
Can you use frozen BAL when working with Chromium Single Cell Gene Expression?
Yes. Dr. Lambrechts and his team used both fresh and frozen BAL fluid for their experiments. Immediately after collection, a portion of the retrieved BAL sample was prepared and subsequently used for scRNA-seq, while the remaining was centrifuged and frozen at −80ºC for later use.
What is the best practice to capture a good amount of cells in the BAL?
The sample processing methods Dr. Lambrechts and his colleagues leveraged included the following steps:
Following retrieval by the performing endoscopist, BAL was separated into two aliquots. The aliquot used for scRNA-seq was immediately put on ice and transported to a BSL-3 laboratory. BAL fluid was centrifuged and the supernatant was frozen at −80°C for further experiments, while the cellular fraction was resuspended in ice-cold PBS. Samples were filtered using a 40 μm nylon mesh. Then, following another centrifugation step, the supernatant was decanted and discarded, and the cell pellet was resuspended in red blood cell lysis buffer. After a 5-minute incubation period at room temperature, the samples were centrifuged and resuspended in PBS containing UltraPure BSA and filtered over Flowmi 40 μm cell strainers using wide-bore 1 mL low-retention filter tips. These steps were followed by cell counting to determine the concentration of live cells.
For more general guidelines on processing BAL, please refer to this literature, Translational Research in Pediatrics III: Bronchoalveolar Lavage.
Investigating the cellular composition of BAL from COVID-19 patients
Were barcoded antibodies used to identify various cell populations?
No. Dr. Lambrechts explained that, though he and his team would usually have a pool of barcoded antibodies with which they would incubate the cells, in this case, the conditions of the experiment did not allow for it. Because of the high-containment requirements for SARS-CoV-2 experiments they chose not to add barcodes. However, Dr. Lambrechts noted that barcoded antibodies are very useful in other circumstances. He has, for example, used these antibodies to confirm markers at both the RNA and protein levels in other experiments.
How much of the T-cell response is antigen-driven versus the result of bystander activation due to hyper inflammation? Since exhaustion is antigen-non-specific, could T cells specific to other antigens be depleted?
While acknowledging that scRNA-seq data isn’t sufficient to fully answer the question, Dr. Lambrechts offered some ideas, hypothesizing the antigen specificity of two T-cell populations. In one case, along the trajectory of CD8+ resident memory T cells, Dr. Lambrechts and his team saw a drop in TCR richness, suggesting that these cells are antigen-specific. However, the trajectory of exhausted T cells did not demonstrate a drop in richness but did display signs of stress, especially in patients with critical COVID-19, suggesting that this population is antigen-non-specific.
To capture neutrophils, you had to decrease the minimum number of genes required by your filtering settings. Does that increase the amount of noise from empty droplets?
Dr. Lambrechts and his colleagues noticed a stark difference in the number of neutrophils detected when adjusting their filtering settings. When set to filter out cells with fewer than 200 genes expressed, they observed very few neutrophils, but after loosening their settings to only filter out cells with fewer than 150 genes expressed, they saw a nearly 5-fold increase in the number of neutrophils. Looking at previously published COVID-19 studies, which suggested that neutrophils play an important role in the disease, they decided to use the less stringent filtering and study the larger neutrophil population. To help ensure their results were coming from actual neutrophils and not empty droplets, they used an extensive set of neutrophil marker genes. They then compared these markers to several published scRNA-seq datasets to verify their reliability. During the experiment, they found neutrophils to be significantly enriched in COVID-19 BAL samples and confirmed the presence of multiple neutrophil marker genes.
Is ACE2 receptor expressed in certain immune cell subtypes? Could SARS-CoV-2 be modulating T-cell markers used to classify the T-cells upon infection?
Dr. Lambrechts and his colleagues did not find evidence of ACE2 receptor expression in immune cells. Instead, their data suggests that ACE2 receptors are expressed in epithelial cells, which led them to propose that SARS-CoV-2 infects epithelial cells as its primary target.
Review the on-demand webinar for more details on this COVID-19 study. If you have any further questions regarding sample prep for single cell gene expression, explore demonstrated protocols and technical notes on our support site—including an FAQ for processing samples with infectious agents—or contact us at support@10xgenomics.com.
Finally, learn more about how 10x Genomics technology is being used to study COVID-19 and other infectious diseases with these resources.
