Revealing drug targets for ovarian cancer with single cell RNA sequencing
*Impact at a glance: Scientists used the Universal 5' Gene Expression assay, previously known as Chromium Single Cell Immune Profiling, to characterize the tumor–immune cell composition in 14 individuals with advanced ovarian cancer and varying responses to chemotherapy. They discovered a population of ascites-derived GZMK+ CD8+ effector memory T cells associated with better cancer prognosis, concluding that manipulating these cells by accelerating their migration into tumor sites could improve therapeutic outcomes.*
Ovarian cancer is a rare disease—about 1.3% of all women will be diagnosed with it in their lifetime—but it’s still the fifth leading cause of cancer-related deaths in women (1). Most women aren’t diagnosed until the cancer has significantly progressed and metastasized to other parts of the body. Less than 50% of women survive five years after their initial diagnosis.
But treatment options for people with ovarian cancer are improving—the FDA has approved more drugs since 2014 than it did in the 60 years prior (2). Unfortunately, like most cancer treatments, treatment efficacy and toxicity varies significantly between people. For example, mirvetuximab soravtansine-gynx received accelerated approval in 2022, but only for patients with “folate receptor alpha (FRα) positive, platinum-resistant epithelial ovarian, fallopian tube, or primary peritoneal cancer, who have received one to three prior systemic treatment regimens” (3).
Single cell RNA sequencing, however, helps researchers understand how cellular heterogeneity contributes to mechanisms of drug efficacy and toxicity by uncovering rare cell populations and discrete cell states.
Recently, a group of researchers used our Chromium Single Cell Immune Profiling assay to develop a comprehensive atlas of the tumor microenvironment of primary tumors, metastases, and ascites—excess fluid buildup in the abdomen due to pressure from tumors commonly seen in people with an advanced stage of cancer that has spread to the abdomen (4). They identified unique cell subclusters enriched in ascites associated with positive immunotherapy and chemotherapy responses.
Notably, they discovered a population of tumor-infiltrating lymphocytes (TILs) in ascites that may migrate to and strengthen the immune response in primary tumors and metastases.
“Our work on ascites-enriched T cells inspires us to rethink the functions of malignant ascites in shaping the tumor microenvironment,” the authors wrote in the recently published Nature Cancer study.
Unraveling the T-cell response to ovarian cancer tumors
To study the relationship between tumors, metastases, and ascites, the researchers examined samples from patients with high-grade serous ovarian cancer (HGSOC)—the most common type of ovarian cancer, accounting for 70% of all cases. 75% of people already have widespread metastases and ascites once they are diagnosed. And effective treatment options are limited.
Immunotherapies are effective for some patients—nearly 10% of 125 patients previously treated with chemotherapy responded to avelumab in a phase 1b clinical trial (5). Researchers attribute varied immunotherapeutic responses to differences in how many TILs effectively invade the primary tumor and its metastases.
For example, last year, researchers from the Moffitt Cancer Center study used our Chromium Single Cell Immune Profiling and our Single Cell Multiome ATAC + Gene Expression assays to analyze 83,454 tissue-resident memory T cells from 122 HGSOC tumors (6). They validated that ovarian cancer is an immunogenic disease—3% of total T-cell receptors (TCRs) in CD8+ T cells from tumors recognized ovarian cancer antigens—and, therefore, should be responsive to immunotherapies despite low response rates observed in clinical trials.
But why these tumors rarely respond to immunotherapy isn’t clear.
Rethinking the role of ascites in shaping the ovarian cancer TME
Researchers think the ascites-enriched T cells may play a critical role in the immune response to ovarian cancer tumors, and provide a path to improving immunotherapy responses in these tumors.
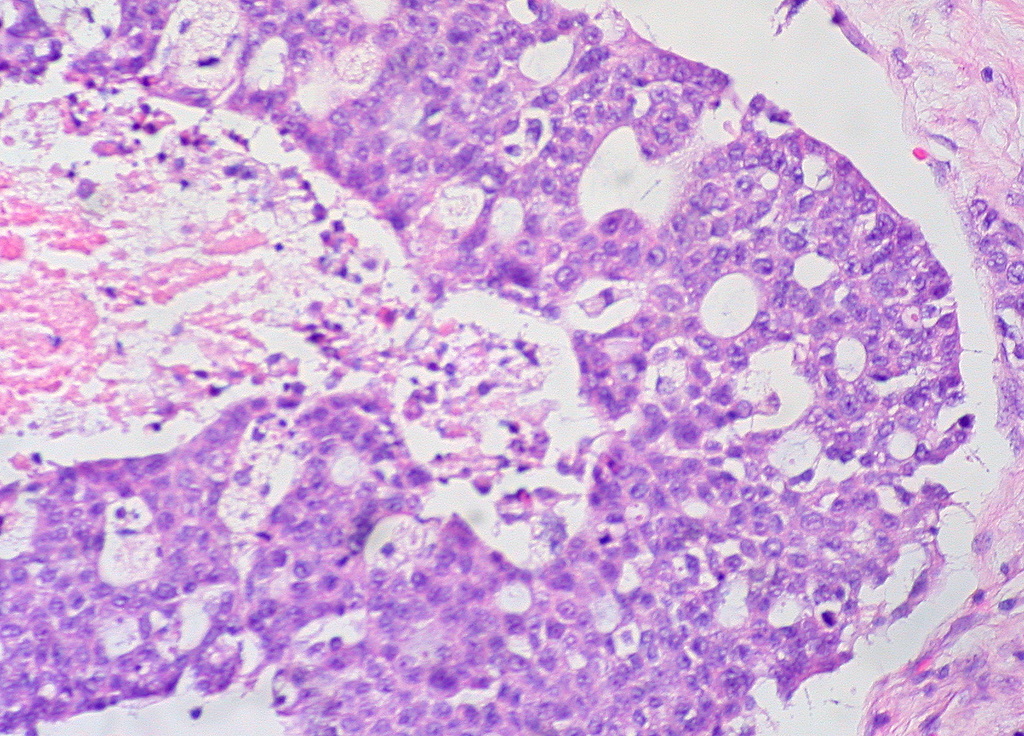
In the Nature Cancer study published in July, the scientists used the Chromium Single Cell Immune Profiling assay to compare immune cellular compositions of five separate tumor-related sites—including primary ovarian tumors, omentum metastases, ascites, pelvic lymph nodes, and peripheral blood—from 14 patients with advanced ovarian cancer with varying responses to chemotherapy. They categorized cells, based on canonical gene expression markers, into five major cell lineages: lymphoid cells, myeloid cells, stromal cells, endothelial cells, and cancer cells.
As expected, primary tumors and their metastases had the same, basic cellular makeup; pelvic lymph nodes were enriched with B cells and CD4+ T cells; peripheral blood contained lymphocytes and monocytes.
Ascites had large numbers of stromal and immune cells, particularly CD8+ T cells, macrophages, and dendritic cells, which represent the classic makeup of an inflammatory environment. All ascites samples also contained cancer cells.
The researchers took a closer look at the T-cell populations in samples from patients with HGSOC. Using unsupervised clustering, they identified five CD4+ clusters, five CD8+ clusters, and two unconventional clusters. A cluster of CD8+ effector memory T cells highly expressing the gene-expressing protease granzyme K (GZMK) was highly enriched in astrocytes. Interestingly, previous studies found that lung cancer tumors enriched with these GZMK+ T cells responded better to immunotherapy.
Further analysis using the TCR-tracking algorithm STARTRAC revealed that ascites-derived GZMK+ T cells shared TCR sequences with exhausted T cells in primary tumors and metastases. This suggests that these cells likely infiltrate tumors where they then differentiate into exhausted T cells.
The authors suggest that, since high levels of GZMK+ T cells are found in lung cancer tumors associated with better lung cancer prognosis, manipulating these cells in patients could improve outcomes in ovarian cancer patients.
“As reported, pre-exhausted GZMK+ T subpopulations were regarded as pre-activated T cells which would accumulate in responsive lung cancer and melanoma tumors following immune-checkpoint-based treatment. We suspected that accelerating the migration of ascites-derived [GZMK+ CD8+ effector memory T cells] into tumor sites could be a potential therapeutic strategy for [ovarian cancer],” wrote the authors.
Further studies clarifying the function of this unique cell population in ovarian cancer samples and beyond could help researchers better understand varied immunotherapy responses in a variety of tumors.
Explore how our Chromium Single Cell Immune Profiling assay can help you identify novel immune cell populations in your samples.
References:
- https://www.aacr.org/patients-caregivers/awareness-months/ovarian-cancer-awareness-month/
- https://ocrahope.org/news/2022-breakthroughs-in-ovarian-cancer-research-and-treatment/#:~:text=Ovarian%20cancer%20immunotherapy&text=Some%20monoclonal%20antibodies%20are%20considered,cells%20to%20kill%20cancer%20cells.
- https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-mirvetuximab-soravtansine-gynx-fra-positive-platinum-resistant
- Zheng X, et al. Single-cell analyses implicate ascites in remodeling the ecosystems of primary and metastatic tumors in ovarian cancer. Nat Cancer 4: 1138–1156 (2023). doi: 10.1038/s43018-023-00599-8
- Disis ML, et al. Efficacy and Safety of Avelumab for Patients With Recurrent or Refractory Ovarian Cancer Phase 1b Results From the JAVELIN Solid Tumor Trial. JAMA Oncol 5: 393-401 (2019). doi:10.1001/jamaoncol.2018.6258
- Anadon CM, et al. Ovarian cancer immunogenicity is governed by a narrow subset of progenitor tissue-resident memory T cells. Cancer Cell 40 (5): P545-557.E13 (2022). doi: 10.1016/j.ccell.2022.03.008
