Single cell analysis of CD19 CAR T-cell therapy for large B-cell lymphomas may help predict efficacy and toxicity
From February 8–12, 2021, 10x Genomics will host a Global Cell Therapy Virtual Symposium, which will gather leading immuno-oncology scientists to discuss their research using single cell techniques. In this blog post, we describe work from the lab of Michael Green, PhD, who is one of the event’s featured speakers. His lab recently published research that used single cell technologies to study the infusion products of patients undergoing CD19 CAR T-cell therapy for large B-cell lymphomas, and how specific cell phenotypes might be predictive of efficacy and toxicity.
To further our understanding of how to create better cell and gene therapies, 10x Genomics will host a Global Cell Therapy Virtual Symposium, to be held February 8–12, 2021, that will gather the global community of researchers in the cancer immunotherapy space. While significant strides have been made in developing cell therapies to treat cancer, scientists continue to advance understanding of how to deepen efficacy and reduce toxicity of these treatments. They are using single cell technologies to push boundaries, and this symposium will feature new insights in cell therapy biology and avenues for designing and optimizing next-generation therapies.
In an effort to promote some of the most promising research in the field of cancer immunotherapy, we are highlighting published work from the lab of Michael Green, PhD, Associate Professor, Division of Cancer Medicine, The University of Texas MD Anderson Cancer Center, who is a featured speaker at the upcoming symposium. Dr. Green’s lab used 10x Genomics single cell RNA-sequencing (scRNA-seq) to further our understanding of why certain patients show poor response or develop toxicities after treatment with CD19 CAR T-cell therapy for large B-cell lymphomas (LBCLs).
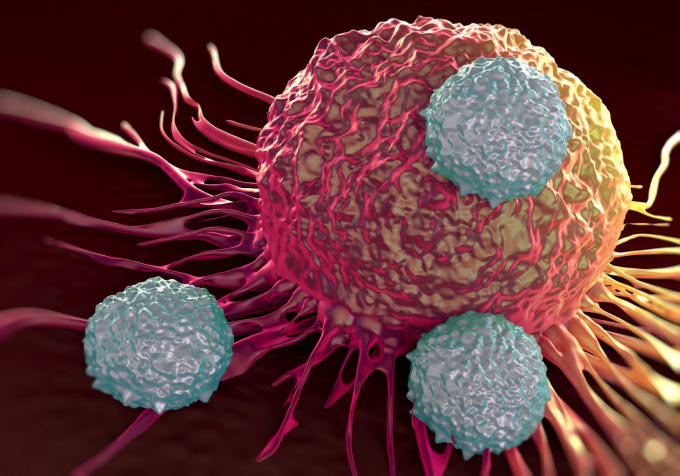
While checkpoint inhibitors and monoclonal antibodies have shown success for treating some types of cancer, one of the most promising immunotherapies is chimeric antigen receptor (CAR) T-cell therapy. However, some challenges persist in the development of this therapy, including resolving the mechanisms behind variable patient response, treatment resistance, and toxicities—which remain a critical focus of ongoing research.
Single cell picture of infusion product resolves difference in treatment response
One type of CAR T-cell therapy targets CD19, a protein located on the surface of B cells. When targeted to the CD19 antigen, this therapy can treat B-cell cancers like leukemia, lymphoma, and multiple myeloma. Even though CD19-directed CAR T-cell therapy is effective for treating LBCL, less than 50% of patients experience long-term remission of their cancer while some patients develop adverse reactions, such as cytokine release syndrome and immune effector cell–associated neurotoxicity syndrome (ICANS). In adults treated with CAR T, ICANS is more commonly high-grade, with 30–45% of patients developing the high-grade (severe) toxic reaction to treatment.
In a study published in Nature Medicine, “Characteristics of Anti-CD19 CAR T Cell Infusion Products Associated with Efficacy and Toxicity in Patients with Large B Cell Lymphomas,” Dr. Green and his team showed that treatment response could be predicted within the first week of therapy, and they discovered a monocyte-like rare cell population that could be associated with the development of ICANS. If clinicians can quickly identify patients who might experience less efficacy and adverse treatment reactions, they could more quickly respond by changing treatment or reducing toxic side effects.
Dr. Green’s lab hypothesized that differences among CAR T cells—specifically, functional heterogeneity—once infused, might be the reason some patients respond better than others to treatment. To resolve the variability in response to CAR T-cell therapy among patients, the researchers compared single cell gene expression patterns of CAR T cells infused into patients. They performed scRNA-seq of 137,326 residual cells after infusion of CAR T cells into 24 patients with LBCL and compared these patterns to treatment responses at a three-month follow-up, post-infusion, with PET/CT scans. In patients who were less responsive to treatment (classified as partial response or progressive disease), they saw an enrichment of exhausted T cells in the infusion product while patients with a complete response to treatment showed a threefold enrichment of memory T cells.
The researchers also found that they could predict long-term outcome of therapy by measuring early molecular response from one week up to one month after infusion. By analyzing plasma-derived, cell-free DNA at one week, two weeks, and one month after treatment, they found that patients who responded within the first week of treatment were more likely to have a complete response. When the group compared cellular functional states within infusion products to early molecular response, they also discovered an association between T-cell exhaustion signatures and a poor early molecular response.
Monocyte-like cells contribute to development of ICANS
Zeroing in on which T cells in the infusion product could be linked to toxicities, the team made a surprising discovery. After profiling the infusion product by scRNA-seq, they identified a population of cells that were significantly overrepresented in the infusion products of patients who developed high-grade ICANS. This population of cells was characterized by a monocyte-like gene expression signature, making them similar to myeloid cells. They were able to validate these findings within the original cohort plus an additional 16 patients.
The paper’s findings suggest that cellular heterogeneity in the infusion product is at the heart of the difference in patient response to CD19 CAR T-cell therapy for LBCLs. This could inform future CAR T-cell therapy design and manufacturing and offer strategies for therapeutic interventions to improve efficacy in poor responders. In the case of toxicity syndromes like ICANS, identification of cell populations in the infusion product may also alert clinicians to patients who may be at a higher risk of developing serious toxicities.
Learn more about this study and other advances in cancer immunotherapy research at our upcoming 10x Genomics Global Cell Therapy Virtual Symposium.** Register today.**
