Single cell analysis reveals new possible therapy strategies for aggressive and treatment-resistant breast cancers
October is National Breast Cancer Awareness Month in the United States. To help raise awareness, we wanted to profile recent publications that highlight current advances in research toward targeted breast cancer therapies, including studies of HER2-positive and triple negative breast cancers. With the insights provided by single cell RNA-sequencing into the cellular heterogeneity of both tumors and the tumor microenvironment (TME), researchers are gaining a more detailed understanding of why standard-of-care therapies may not be effective for some cancers, how more than one therapy can be combined to improve treatment outcomes, and how certain cells can be pinpointed as therapeutic targets.
Breast cancer is the second leading cause of cancer death in women after lung cancer, and an estimated one in eight women will be diagnosed with breast cancer in their lifetime. Stratification of breast cancer types based on expression of three key genes, estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2), helps guide optimal therapy options. For example, the standard-of-care therapy for HER2-positive (HER2+) breast cancer is herceptin (trastuzumab), an antibody therapy that works by binding to the HER2 receptor on a cell’s surface and blocking the cellular signaling that tells the cell to grow. Herceptin may be used alone or in combination with other therapies, including chemotherapy and immunotherapy, a treatment class that attempts to stimulate the body’s immune system to fight cancer cells.
Triple negative breast cancer (TNBC) expresses none of the usual breast cancer therapeutic targets, including ER, PR, and HER2, making it unresponsive to either hormone therapy or targeted anti-HER2 drugs like trastuzumab. The primary treatment options for patients with TNBC are chemotherapy, surgery, and radiation. TNBC tends to be more aggressive and have poorer prognosis than other breast cancer subtypes, indicating an even greater need for novel targeted treatment options.
In most breast cancers, differences between cells within tumors and within the tumor microenvironment can impact cancer progression but, up until recently, have not been well studied. The following sections will review two recent studies that explore these facets of tumor biology as they pertain to immunity, including how vaccination and immune checkpoint blockade might be combined to improve outcomes for metastatic HER2+ breast cancer, and how immune activity in the TME can be better understood to discover new small molecule drug targets for TNBC.
Combined vaccine and immune checkpoint inhibitor therapy may improve outcomes in HER2+ breast cancer
While PD-1/PD-L1 immune checkpoint inhibitors, a type of antibody-based drug that increases the immune response against tumors, have been shown to be effective in treating certain types of cancer, their efficacy for breast tumors is only beginning to be explored (1). In a study led by Dr. Erika Crosby from Duke University, researchers tested whether a vaccine targeting a specific epitope of HER2—a highly oncogenic form of the protein called HER2delta16—coupled with immune checkpoint inhibitor therapy would improve treatment outcomes in metastatic and/or treatment-resistant HER2+ breast cancer.
Using single cell immune profiling technology to sequence the paired T-cell receptor a/b chains of tumor-infiltrating T cells (TILs) in a mouse model, the team was able to assess clonal expansion and phenotype of HER2-reactive T cells. They found that HER2delta16 vaccination alone resulted in significant—and essential—antitumor CD8+ T-cell activity. However, TILs from vaccine-only mice showed immune dysfunction. As they discovered, it was necessary to use both the vaccine and PD-1 antibody therapy for long-term tumor control of advanced cancers (2).
As this research revealed, adding a vaccine to immune checkpoint inhibitor therapy boosts the effectiveness of these inhibitors in a mouse model. While there are many clinical trials investigating combination therapies for HER2+ breast cancer, it remains to be seen how a specific combination of vaccine and immune checkpoint inhibitor therapy might improve outcomes in patients with HER2+ breast cancer. The successful results of this study have in fact led to a phase II clinical trial (NCT03632941) to investigate how effective a combination treatment of a HER2 vaccine and Keytruda (Merck’s immune checkpoint inhibitor therapy) might be in patients with recurrent or metastatic HER2+ cancers. By combining targeted vaccines with immune checkpoint blockade, the field may be able to develop more effective therapies for these hard-to-treat cancers.
Stromal cell diversity influences how the immune system works against triple negative breast cancer
Cancer-associated fibroblasts (CAFs) play an important role in the TME by influencing many aspects of carcinogenesis, making them potential targets for new therapies to treat advanced breast cancers like TNBC, for which there are no targeted therapies. However, these cells are not well understood, having been shown to both promote and suppress tumors. Single cell studies in mouse models have revealed four subclasses of CAFs. Studies in mice and humans have also shown that development of TNBC can be affected by stromal cells. However, scientists have yet to build a comprehensive atlas of stromal cells in human breast tumors.
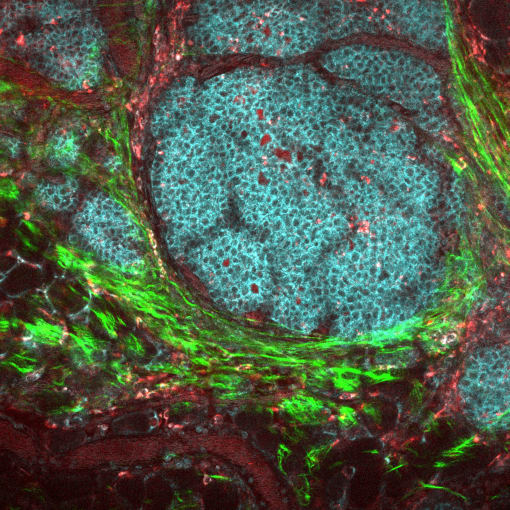
To better understand stromal heterogeneity in TNBC, Dr. Sunny Wu of the Garvan Institute of Medical Research in Australia and team used single cell RNA-seq on breast cancer tissue from five patients to profile the TME. His team found two subpopulations of CAFs and two subpopulations of perivascular-like (PVL) cells. This led them to conclude that these subpopulations perform different functions within the TME. Data analysis from gene signatures of inflammatory CAFs and differentiated PVL cells showed that these cells were strongly associated with cytotoxic T cell (CTL) dysfunction and exclusion, respectively. Normally, CTLs increase the immune response; if they are prevented from reaching the tumor, they are said to be “excluded.”
While immune checkpoint therapies have shown limited efficacy in the treatment of advanced TNBC, this research points to specific CTL immune pathways as possible new therapeutic targets. Moreover, Dr. Wu’s findings suggest that, in a subset of patients, targeting more than one stromal subpopulation could produce a more effective immune response than targeting one subpopulation alone (3).
Better treatments on the horizon for breast cancer
As these studies demonstrate, single cell sequencing technology is moving the field toward being able to better understand and predict cellular heterogeneity and cell-to-cell interactions in breast cancers. Dr. Crosby and her team at Duke have shown that single cell insights in mouse models can readily lead to trials testing promising new combination therapies for HER2+ breast cancers—underscoring the importance of applying cutting-edge tools to translational research. As a result, precision therapies that target specific pathways within cells or multiple pathways simultaneously are on the horizon for the treatment of previously aggressive or treatment-resistant tumors.
References
- G Planes-Laine et al., PD-1/PD-L1 Targeting in Breast Cancer: The First Clinical Evidences are Emerging—A Literature Review. Cancers (Basel). 11 (7), 1033 (2019).
- EJ Crosby et al., Stimulation of Oncogene-Specific Tumor-Infiltrating T Cells through Combined Vaccine and αPD-1 Enable Sustained Antitumor Responses against Established HER2 Breast Cancer. Clin. Cancer Res. 26, 4670–4681 (2020).
- SZ Wu et al., Stromal cell diversity associated with immune evasion in human triple‐negative breast cancer. EMBO Journal. 39, 19 (2020).
