Understanding the T-cell response to personalized cancer vaccines
Intravenous or subcutaneous? Scientists from the Vaccine Research Center at the National Institutes of Health recently demonstrated that location of administration matters when it comes to personalized cancer vaccines. In their comparison of the two vaccination strategies, they identified a stem-like CD8+ T-cell population elicited by intravenous injection that has greater capacity to proliferate and replenish effector T cells, and kill tumor cells in combination with immune checkpoint therapy. Learn how a single cell view of the T-cell response to personalized cancer vaccines supported their conclusions.
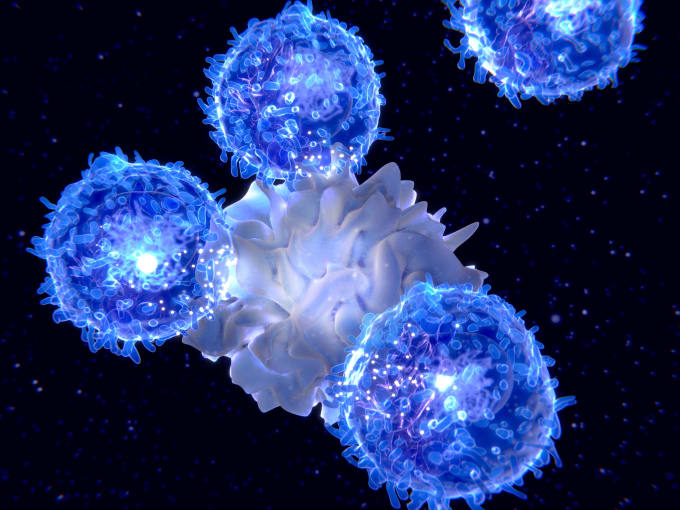
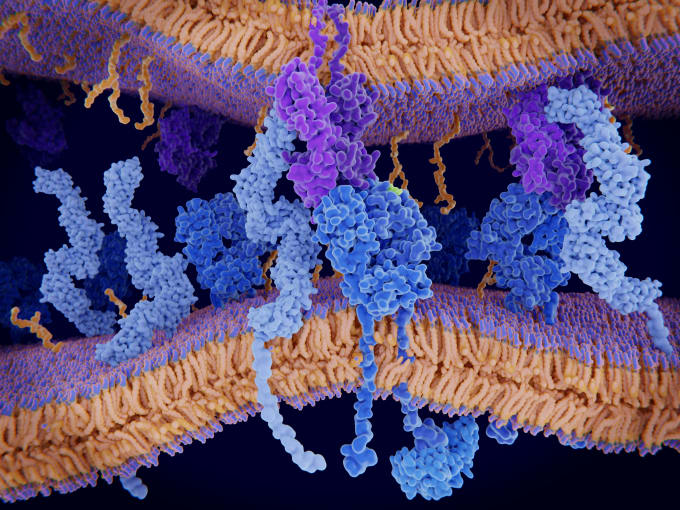
Vaccines can be useful for more than defending us against viruses. Fundamentally, vaccines enable us to prime our immune systems against antigens—that is, exogenous molecular structures that are recognized by immune cells and promote an immune response. T cells are an important contributor to this defensive response. They’re activated when T-cell receptors recognize and bind to antigen-MHC complexes on the surface of antigen-presenting cells. Upon activation, antigen-specific T cells can proliferate and differentiate to take on other defensive roles that protect our bodies from the pathogen that yielded the original antigen. In their development, T cells and other immune players that mediate the immune response to antigens are carefully monitored and trained to avoid reacting with self-antigens, meaning molecular structures derived from our own cells. This ensures that our immune systems do not betray us and focus on targeting foreign pathogens that cause disease. However, what if our own cells—for example, cancer cells—are the source of harm and disease? Can the same principles of vaccination be manipulated to treat cancer?
These questions form the conceptual basis of an emerging field of translational oncology that leverages personalized cancer vaccines to stimulate the immune system against cancer. To avoid autoreactivity, the vaccine approach relies on tumor neoantigens, a repertoire of unique peptides present on the surface of a patient’s cancer cells. Jiang et al. says “From an immunological perspective, [a] tumor neoantigen is the truly foreign protein and entirely absent from normal human organs/tissues. For most human tumors without a viral etiology, tumor neoantigens could derive from a variety of nonsynonymous genetic alterations including single-nucleotide variants, insertions and deletions, gene fusions, frameshift mutations, and structural variants” (1). These neoantigens could be recognized by killer T cells in the body which could then be activated against cancer cells, in much the same way T cells would target virus-infected cells presenting viral antigens. The therapeutic approach culminated in 2014 when six melanoma patients at Washington University School of Medicine in St. Louis were the first people to receive an anticancer vaccine, which was composed of each patient’s own dendritic cells presenting digested cancer peptides derived from their own melanoma tumors. Of three patients the study authors subsequently reported on, none had adverse autoimmune events. In fact, two patients’ cancers remained stable while one patient experienced complete remission in the months following vaccination. Additionally, they were each shown to have a more diverse neoantigen-specific T-cell receptor repertoire, highlighting the potential of cancer vaccines to elicit antitumor immunity (2).
Location matters for personalized cancer vaccines
The promise of this immunotherapy has led scientists to consider how to optimize cancer vaccine platforms, including how to package and deliver cancer peptides, where to inject the vaccine in order to elicit the most effective endogenous T-cell response, and at what optimal dosage to deliver antigen. Dr. Robert A. Seder and researchers from the Vaccine Research Center at the National Institutes of Health are leading the way in this effort. Using a nanoparticle vaccination platform leveraging peptide adjuvants and co-delivery of a Toll-like receptor 7/8 (TLR7/8) agonist to ensure maturation of antigen-presenting cells (3), they sought to understand the differences in efficacy between intravenous and subcutaneous vaccination routes. Is one route more effective at delivering tumor neoantigens to T cells and ultimately notifying the immune system of resident cancer cells to target and destroy?
To test this, the research team vaccinated mice with a murine colon carcinoma neoantigen, Reps1. They quantified T cells in the blood of the mice using a tetramer staining assay—in which Reps1-bound MHC tetramers marked by a fluorophore can label and enable counting of neoantigen-specific T cells via flow cytometry. They observed that subcutaneous administration elicited 20-fold higher neoantigen-specific CD8+ T cells compared to intravenous vaccination. Further annotation of this divergent T-cell response revealed that approximately 60% of neoantigen-specific T cells elicited by subcutaneous vaccination expressed surface markers for short-lived effector cells—T cells that perform cytotoxic killing or other immune activating functions—while 60% of those elicited by intravenous vaccination carried markers of CD8+ memory precursor effector cells—T cells that have not fully differentiated to the effector state, but are sensitive to antigen (4). The full extent of the phenotypic and transcriptional differences between these T-cell populations, and how they came to differentiate based on vaccination route, was still unclear however.
Understanding the T-cell response to cancer vaccines with single cell RNA-seq
These findings confirmed that the route of vaccine administration could influence the type of T cells that were activated in response to tumor neoantigen. In order to more deeply characterize the identities and functional roles of these activated T cells—and determine which response was holistically more effective at producing antitumor immunity—the research team then turned to single cell RNA-sequencing. They collected spleens from another cohort of mice vaccinated either subcutaneously or intravenously, then enriched for antigen-specific CD8+ T cells via tetramer staining and flow cytometry. Differential gene expression analysis revealed 12 distinct T-cell clusters, with clear separation between clusters by vaccination route. T cells elicited by intravenous vaccination showed significant expression of stem cell–like genes, including Tcf7, Slamf6, and Xcl1, as well as genes associated with T-cell exhaustion and anti-apoptotic processes. In contrast, T cells elicited by subcutaneous vaccination showed heightened expression of effector genes like Gzmb, Klrg1, Cx3cr1, and Zeb2, the latter of which is known to trigger cytotoxic T cells to adopt a terminally differentiated state. These insights confirmed that each vaccination route elicited a distinct T-cell response.
In order to determine relative antitumor efficacy, the team next established an in vivo mouse tumor model, treating the mice with vaccine and anti-PD-L1 immune checkpoint therapy. Significantly, they found that though the numbers of neoantigen-specific CD8+ T cells between both vaccination routes were of comparable magnitude, mice injected subcutaneously could not control tumor growth, while mice injected intravenously could and had extended survival. Flow cytometry analysis of the T-cell composition in the spleens of mice collected at day 14 of the treatment program confirmed that the majority of T cells were stem-like after intravenous vaccination. Additionally, at day 21 following intravenous vaccination, spleens taken from the mice had mostly differentiated to effector cells, suggesting the intravenous vaccination had elicited a prolonged antitumor response through stem-like T cells, which could proliferate and replenish effector cells. Why did intravenous vaccination produce these results? The team showed through in vivo imaging that it was likely due to differences in how, and how long, antigen-presenting dendritic cells were primed with antigen. While intravenous vaccination rapidly distributed antigen systemically, subcutaneous vaccination caused antigen to persist in the lymph nodes, driving an antigen-specific T-cell response that ultimately had lower proliferative potential as T cells became terminally differentiated (4).
New clinical implications for personalized cancer vaccines from single cell insights
The efficacy of personalized cancer vaccines, and other cancer immunotherapies, is ultimately determined by the magnitude and quality of the T-cell response. Can T cells infiltrate the tumor microenvironment and target cancer cells with precision? Can they kill the cancer cells effectively over time? Single cell approaches are helping researchers uncover deep insights into these crucial T-cell dynamics and work out clinical variables—from optimal dosage to route of vaccination—that can ensure the best possible results for patients as these new therapies advance to clinical trials, and on to more established treatment programs.
References:
- Jiang T, et al. Tumor neoantigens: from basic research to clinical applications. J of Hem & Onc 12: 93, 2019.
- Carreno BM, et al. A dendritic cell vaccine increases the breadth and diversity of melanoma neoantigen-specific T cells. Science 348: 803–808, 2015.
- Lynn G, et al. Peptide-TLR-7/8a conjugate vaccines chemically programmed for nanoparticle self-assembly enhance CD8 T cell immunity to tumor antigens. Nat Biotechnol 38, 3: 320–332, 2020.
- Baharom F, et al. Intravenous nanoparticle vaccination generates stem-like TCF1+ neoantigen-specific CD8+ T cells. Nat Immunol 22, 1: 41–52, 2020.
