Can single cell genomics help us crack the epigenetic code underlying vaccination and immunity?
National Immunization Awareness Month (NIAM) is observed each year during the month of August to underscore the importance of vaccinations. As a tool for immunization, vaccines are important in preventing serious and sometimes fatal diseases in people of all ages.
In light of the current COVID-19 pandemic, vaccines have become a hot topic of discussion. While there are several vaccines available to the public—all of which have been proven to protect against serious disease—many people choose to remain unvaccinated. NIAM hopes to raise awareness about the important role that vaccines play in preventing serious disease and population outbreaks. In this post, we take a look at a recent study that utilized a combination of single cell profiling tools to map the epigenomic landscape underlying the efficacy of the influenza vaccine.
Vaccines are foundational to both individual and public health
Through immunizations, some diseases have been almost completely eradicated, one example being polio. In fact, vaccination has been named one of the “Ten Great Public Health Achievements” of the past century (1). A vaccine is composed of a weakened or dead form of an infectious pathogen, a surface protein, or some other singular piece of the whole. When it is presented to a person’s immune system (by way of a shot, for example), the vaccine stimulates the body to recognize the foreign substance and create molecules (antibodies) that will recognize it in the future and clear it from the body.
One of the most common seasonal infections comes from the influenza virus; every year, a new vaccine is manufactured with the aim of preventing severe disease and community-based spread. And, while the flu vaccine is effective, less well understood are the immune system factors that contribute to variable levels of individual resistance to infection and disease. A 2012 meta-analysis review revealed that while the flu vaccine was effective 67% of the time, it benefited certain groups of people more than others (2). Interestingly, the influenza vaccine can decrease the severity of illness of multiple flu strains, and it also appears to protect against unrelated illness, such as myocardial infarction (3).
It is with this in mind that scientists are using single cell analysis to peer more closely into the immune response behind vaccination, in general. Tracking what’s happening within cells at the transcriptomic and epigenomic levels will lend increased understanding to how vaccines work on the immune system—and highlight their multifactorial importance (as in, they not only protect against viral variants, but they prime the immune system to protect against different diseases altogether). Despite having studied and identified transcriptional, metabolic, proteomic, and cellular factors that affect vaccine response, the epigenomic landscape remains unknown. In a recent study, scientists led by Florian Wimmers, PhD, in the Stanford University lab of Bali Pulendran, PhD, applied single cell tools to study how influenza vaccination alters the human epigenome in lasting ways (4).
Flu vaccine leads to global epigenomic reprogramming of immune cells
Recent studies have shown that vaccination with live, attenuated bacillus Calmette–Guerin (BCG) leads to epigenomic changes in monocytes (5, 6) that may result in a lasting state of innate immune activation, or a sort of immunological memory. It’s not very well understood, however, as to whether this “epigenomic imprinting” happens with other vaccines.
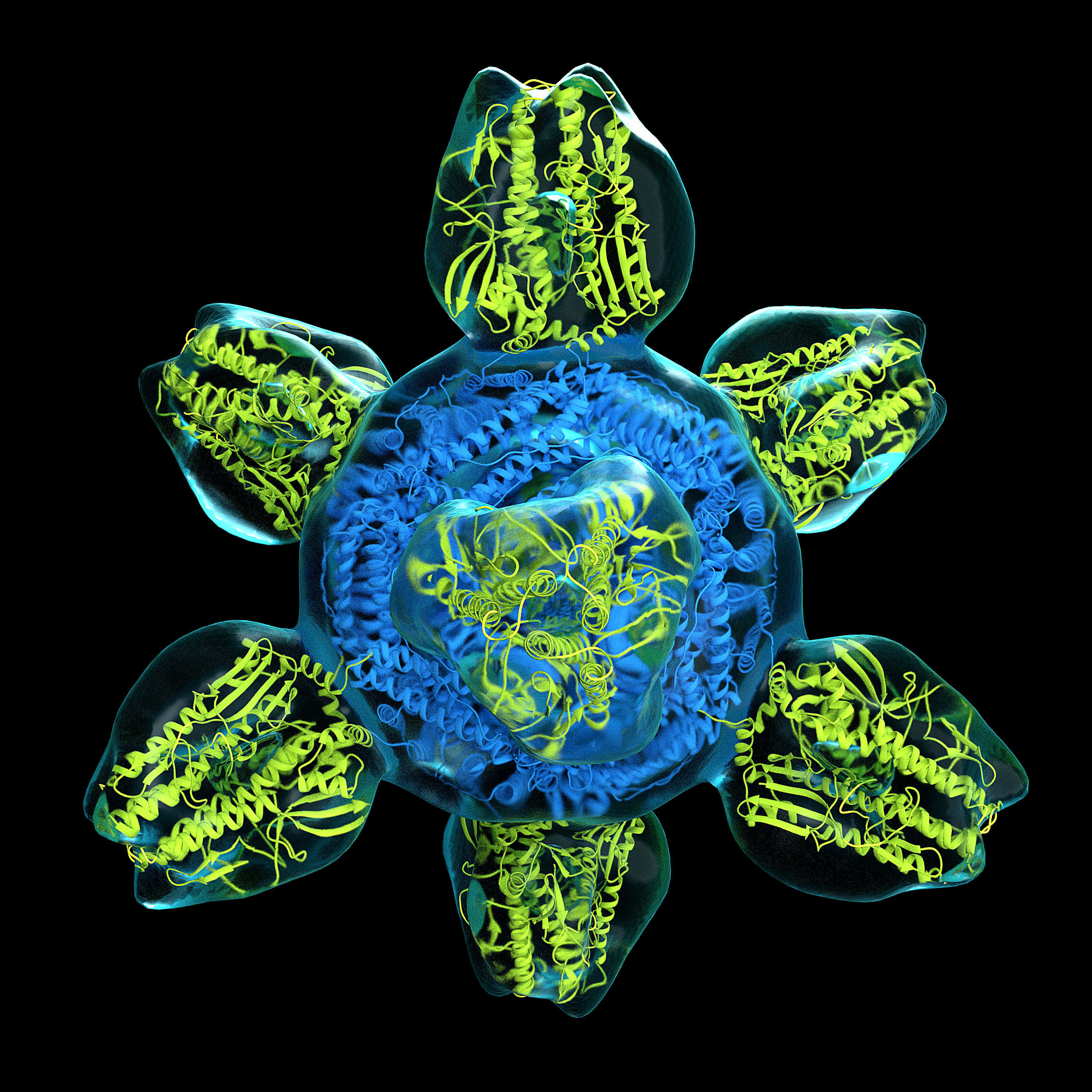
Using a combination of single cell RNA sequencing (scRNA-seq) and single cell assay for transposase-accessible chromatin using sequencing (scATAC-seq), Dr. Wimmers and team created a transcriptomic and epigenomic atlas of immunity to influenza vaccination. After vaccinating a cohort of 21 people aged 18 to 45 with the trivalent inactivated seasonal influenza vaccine (TIV), they profiled chromatin state using Chromium Single Cell ATAC before and after vaccination (in total, 62,101 cells). Following, they performed transcriptomic profiling before and after vaccination using Single Cell Gene Expression (in total, 34,368 transcriptomes). Combined, their data revealed that vaccination led to global chromatin changes in more than one immune cell subtype (but most pronounced in myeloid cells), and that these changes lasted at least six months.
Further analysis revealed that, by day 30 post-vaccination, accessibility of the transcription factor (TF) activator protein 1 (AP-1) was strongly reduced in some cell types, specifically classical monocytes and myeloid dendritic cells. Interestingly, this reduction began on day 1 post-vaccination, which suggested to them that imprinting happens very early in the vaccine response.
At the transcriptomic level, they saw reduced expression of multiple AP-1 family members, including ATF3, JUND, JUNB, FOS, and FOSL2. AP-1 regulates genes that respond to cytokines, growth factors, stress, and bacterial and viral infections.
Because they were surprised that the inactivated seasonal flu vaccine led to decreased TF activity (a type of “trained tolerance,” they labeled it) whereas a live attenuated BCG vaccine showed enhanced and persistent responses (called ‘‘trained immunity’’), they reasoned that BCG vaccine was acting like a vaccine plus adjuvant (something added to the vaccine to aid in activation of the immune response). So, in the next part of their study, they decided to test their hypothesis using a bird flu vaccine plus adjuvant.
Vaccine plus adjuvant leads to both chromatin changes and increased resistance to other viral infections
As adjuvant, they used AS03, a “squalene-based adjuvant containing alpha-tocopherol that induces strong innate and adaptive immune responses" (7). This type of vaccine is also being developed for COVID-19 (8).
Using scATAC-seq and scRNA-seq on PBMC samples from four vaccinated individuals (2 H5N1, 2 H5N1+AS03) at days 0, 21, and 42, they found similar effects as with TIV, which was a significant reduction in AP-1 accessibility in H5N1+AS03 but not H5N1 alone. Notably, the vaccine with adjuvant led to increased chromatin accessibility at interferon response factor (IRF) and signal transducer and activator of transcription (STAT) loci in multiple innate immune cell subtypes, which was also associated with increased expression of antiviral genes. When PBMCs were infected with Dengue or Zika virus, the team saw a significant reduction in viral titers for both viruses at day 21 and, in many cases, as late as 42 days after initial vaccination—pointing to increased resistance to unrelated viruses.
Future focus: Vaccines that offer protection against multiple infectious pathogens
In conclusion, their data suggest that vaccination with an AS03-adjuvanted avian influenza vaccine can and does effect longer-term epigenomic changes in myeloid cells, which leads to an antiviral state and protection against other viruses. Very recently published research out of the same lab of Dr. Pulendran led by Prabhu Arunachalam, PhD, used single cell transcriptomic analysis to demonstrate that two shots of the Pfizer-BioNTech mRNA vaccine led to a subset of myeloid cells with a profile similar to the H5N1+AS03 (reduced AP-1 accessibility and increased expression of interferon genes)—suggesting that this type of vaccine can, indeed, prime the innate immune system to respond even more strongly following a booster shot (9). Ultimately, it may be possible to design new vaccines—whether those with adjuvants or mRNA-based ones—to provide broader protection from variants or other, unrelated viruses.
References:
- https://www.cdc.gov/mmwr/preview/mmwrhtml/00056796.htm
- Osterholm MT, et al. Efficacy and effectiveness of influenza vaccines: a systematic review and meta-analysis. Lancet Infect Dis 12(1): 36–44, 2012. doi: 10.1016/S1473-3099(11)70295-X
- MacIntyre CR, et al. Influenza vaccine as a coronary intervention for prevention of myocardial infarction. Heart 102(24): 1953–1956, 2016. doi: 10.1136/heartjnl-2016-309983
- Wimmers F, et al. The single-cell epigenomic and transcriptional landscape of immunity to influenza vaccination. Cell 184(15): 3915–3935.e21, 2021. doi: 10.1016/j.cell.2021.05.039
- Arts RJW, et al. BCG vaccination protects against experimental viral Infection in humans through the induction of cytokines associated with trained immunity. Cell Host Microbe 23: 89–100, 2018. doi: 10.1016/j.chom.2017.12.010
- Kleinnijenhuis J, et al. Bacille Calmette-Guerin induces NOD2-dependent nonspecific protection from reinfection via epigenetic reprogramming of monocytes. Proc Natl Acad Sci USA 109: 17537–17542, 2012. doi: 10.1073/pnas.1202870109
- Pulendran B, Arunachalam PS, and O'Hagan DT. Emerging concepts in the science of vaccine adjuvants. Nat Rev Drug Discov 20(6): 454–475, 2021. doi: 10.1038/s41573-021-00163-y
- Arunachalam, PS, et al. Adjuvanting a subunit COVID-19 vaccine to induce protective immunity. Nature 594(7862): 253–258, 2021. doi: 10.1038/s41586-021-03530-2
- Arunachalam PS, et al. Systems vaccinology of the BNT162b2 mRNA vaccine in humans. Nature, 2021. Online ahead of print. doi: 10.1038/s41586-021-03791-x
