Investigating the plaque microenvironment in Alzheimer’s disease with spatial gene expression
Extracellular amyloid beta, intracellular tau protein deposits, and neuronal loss represent the classical hallmarks of Alzheimer’s disease. However, scientists are well aware that pathways involving non-neuronal brain cells are also dysregulated throughout the course of disease and likely play an important role in disease pathogenesis. In a recent study, scientists leveraged spatial gene expression approaches to study the molecular pathology of this degenerative brain disease, revealing key molecular changes and cellular interactions within a network of glial cells in the vicinity of amyloid plaques. Read more to learn how spatial analysis is opening up new insights into the cellular contribution of glia to inflammation and overall disease progression in AD.
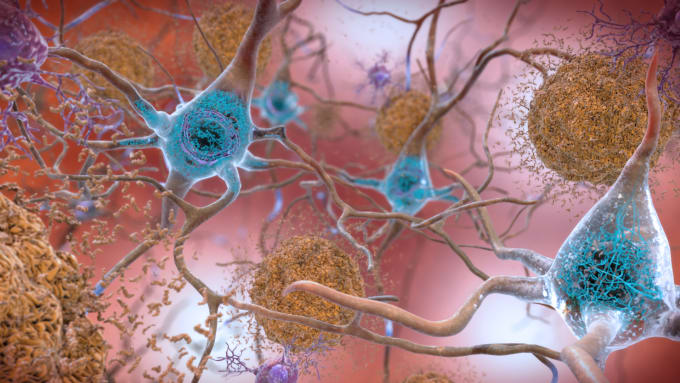
Alzheimer’s disease (AD) is a degenerative brain disease that leads to neuronal loss and behavioral symptoms such as dementia and other forms of cognitive decline. AD is associated with two types of abnormal protein deposits, amyloid beta (Aβ) and tau. While it’s known that buildup of these proteins around and within neurons—Aβ forms sticky plaques around neurons while tau leads to tangles inside nerve cells—is associated with nerve cell damage and death, scientists are questioning assumptions that these proteins are the most productive therapeutic targets for AD. Clinical trials testing anti-amyloid drugs continue to fail to improve the symptoms of cognitive decline, suggesting that clearing plaque alone doesn’t address the full, underlying biological basis of disease—and perhaps, more effective drug targets may be found in an investigation of other pathways involving dysregulated non-neuronal brain cells.
While postmortem anatomical studies can teach us about what brains look like after they’ve been ravaged by AD, single cell and spatial studies untangling the cellular heterogeneity and spatial coordination between neurons and other brains cells within the plaque microenvironment can give insight into the pathways that might be targeted alternatively or earlier in the disease process.
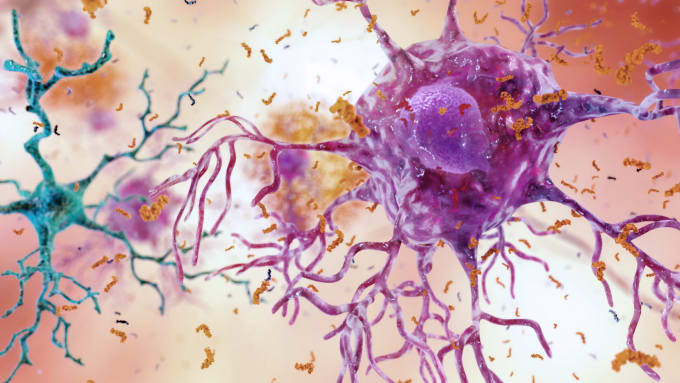
Microglia are one type of non-neuronal brain cells that have been reported to play a key role in AD onset and progression. Recently, we featured research in a blog post that used single cell techniques to build detailed cellular-molecular maps to characterize the role that non-neuronal cells of the hippocampus might play in AD as well as how expression changes in a variant of a microglial receptor, triggering receptor expressed on myeloid cells 2 (TREM2), are associated with increased risk of AD.
While inflammation occurs in the vicinity of amyloid plaques, primary causation is uncertain and little is known about the molecular changes and cellular interactions that characterize this response. In this blog post, we’ll take a look at a recent study that combined spatial transcriptomics (ST) (1) and in situ sequencing on mouse and human AD brain samples, bridging the gap between single cell transcriptomic analysis of non-neuronal cells in AD and their spatial information (2).
Uncovering plaque-induced gene expression networks in Alzheimer’s disease
Scientists led by Drs. Bart de Strooper and Mark Fiers at VIB-KU Leuven Center for Brain & Disease Research in Belgium found two gene co-expression networks that are initiated in response to accumulating amyloid plaques, a plaque-induced gene (PIG) network mainly involving microglia and astroglia and an oligodendrocyte gene (OLIG) network involving myelination genes.
The authors performed ST on tissue sections of AD mouse model brains (at 3, 6, 12, and 18 months) from tissue domains within a 100-micrometer diameter around amyloid plaques. From 10,327 transcriptomic profiles, they were able to characterize two gene co-expression networks resulting from Aβ deposits. (Genes in different cells with similar expression patterns, or co-expression, are likely to have similar functions.) The 57 plaque-induced genes (PIGs) are a response that spans different cell types but mainly involves microglia and astroglia. PIGs include complement, endosomes and lysosomes, oxidation-reduction, and inflammation genes. A second network, oligodendrocyte genes (OLIGs), showed high expression of myelination genes and were mainly expressed by oligodendrocytes. They confirmed these changes at the single cell level with spatial context, using in situ sequencing on mouse and human brain sections.
Considering that PIG expression results in astroglial activation near amyloid plaques and dysregulation of the classical complement cascade, this signaling pathway is a likely drug target. OLIG expression increases activity of myelin-related genes of oligodendrocytes, implicating these cells as possible targets as well.
Looking to the plaque microenvironment for new therapeutic targets
It’s apparent that Aβ is only part of the story of what drives AD, and there are many genes and pathways involving the non-neuronal brain cells surrounding Aβ plaques that might point to larger clues for drug discovery. As scientists continue to unravel the molecular basis for AD, transcriptomic techniques that allow for the integration of spatial context and single cell resolution seem most promising in helping to uncover key cell-to-cell interactions driving AD progression.
You can review this study in more detail by watching a presentation from principal investigator Dr. Bart de Strooper, showcased at the Global Neuroscience Virtual Symposium hosted by 10x Genomics. Explore the symposium offerings to learn how single cell and spatial analysis tools are helping neuroscientists untangle the mechanisms of neurodegenerative diseases. Learn more.
References:
- PL Stahl et al., Visualization and analysis of gene expression in tissue sections by spatial transcriptomics. Science. 353, 78–82 (2016).
- WT Chen et al., Spatial Transcriptomics and In Situ Sequencing to Study Alzheimer's Disease. Cell. 182 (4), 976–991 (2020).
