Young immune systems make fighting COVID child’s play
The Cootie Shot game—often accompanied by the chant "Circle circle, dot dot, now you've got a cootie shot!"—has been played across the United States for generations to ward off germs, usually imaginary, harbored by classmates (1). Although the children playing may not realize it, their immune systems are already hard at work learning to protect them from some genuine threats, including COVID.
In February 2022, the American Academy of Pediatrics (AAP) reported that over 12 million children under 19 years old have tested positive for COVID-19 since the onset of the pandemic (2). Despite high infection rates, the vast majority of children present with relatively mild COVID-19 severity (3). Furthermore, SARS-CoV-2 infections in children account for less than 0.1% of global COVID-19 mortalities (4).
What accounts for the decreased COVID-19 severity experienced by pediatric patients? A consortium of researchers spanning the United Kingdom, Japan, and the United States came together to better understand exactly this. In their study, published in Nature, single cell gene expression enabled the identification of multiple mechanisms that may contribute to the differences observed between pediatric and adult immune responses to SARS-CoV-2 infections (5).
Single cell analysis reveals insights into the aging airway and immune system
To understand the cellular landscape of the airways and immune system following SARS-CoV-2 infection, single cell RNA-sequencing was performed on samples taken from 19 pediatric and 19 adult patients experiencing COVID-19 with varying degrees of severity, and 30 healthy pediatric and 11 healthy adult patients. In all, a dataset of 236,997 cells derived from airway brushings (nose, trachea, and bronchi) and 422,220 cells derived from blood was generated from this cohort of patients.
When examining gene expression changes in airway samples profiled with Chromium Single Cell 5’ and 5’ V(D)J assays, the researchers noted astounding differences between children and adults when it came to interferon (IFN) signaling. Particularly, an activated interferon-alpha (IFNɑ) response was present in the nasal epithelial cells of healthy pediatric patients, such that only a modest increase in expression levels was seen in children after SARS-CoV-2 infection. However, the nasal immune cells of pediatric patients with COVID-19 showed a much stronger induction of the interferon response signature than observed in adults with COVID-19. The authors note that this preactivated epithelial cell and stronger immune cell response in children may contribute to better protection against SARS-CoV-2.
The researchers also performed multiomic profiling on blood samples using Chromium Single Cell V(D)J assay with Feature Barcode technology to explore the circulating immune landscape. This analysis revealed that, in adults with COVID-19, the circulating immune system has a high abundance of cytotoxic T lymphocytes and effector memory cells, indicative of a more systemic infection. In pediatric patients who have COVID-19, there are reduced levels of natural killer cells and CD4+ cytotoxic T lymphocytes, but high numbers of naive lymphocytes.
The authors note that “not only do children have a more naive and reduced cytotoxic response to COVID-19, but they also start off with an immune state that is already skewed towards this response.” As a consequence of having more naive immune cells, younger individuals have higher T-cell receptor (TCR) repertoire diversity, while older patients have more expanded clones.
Learning from our youth
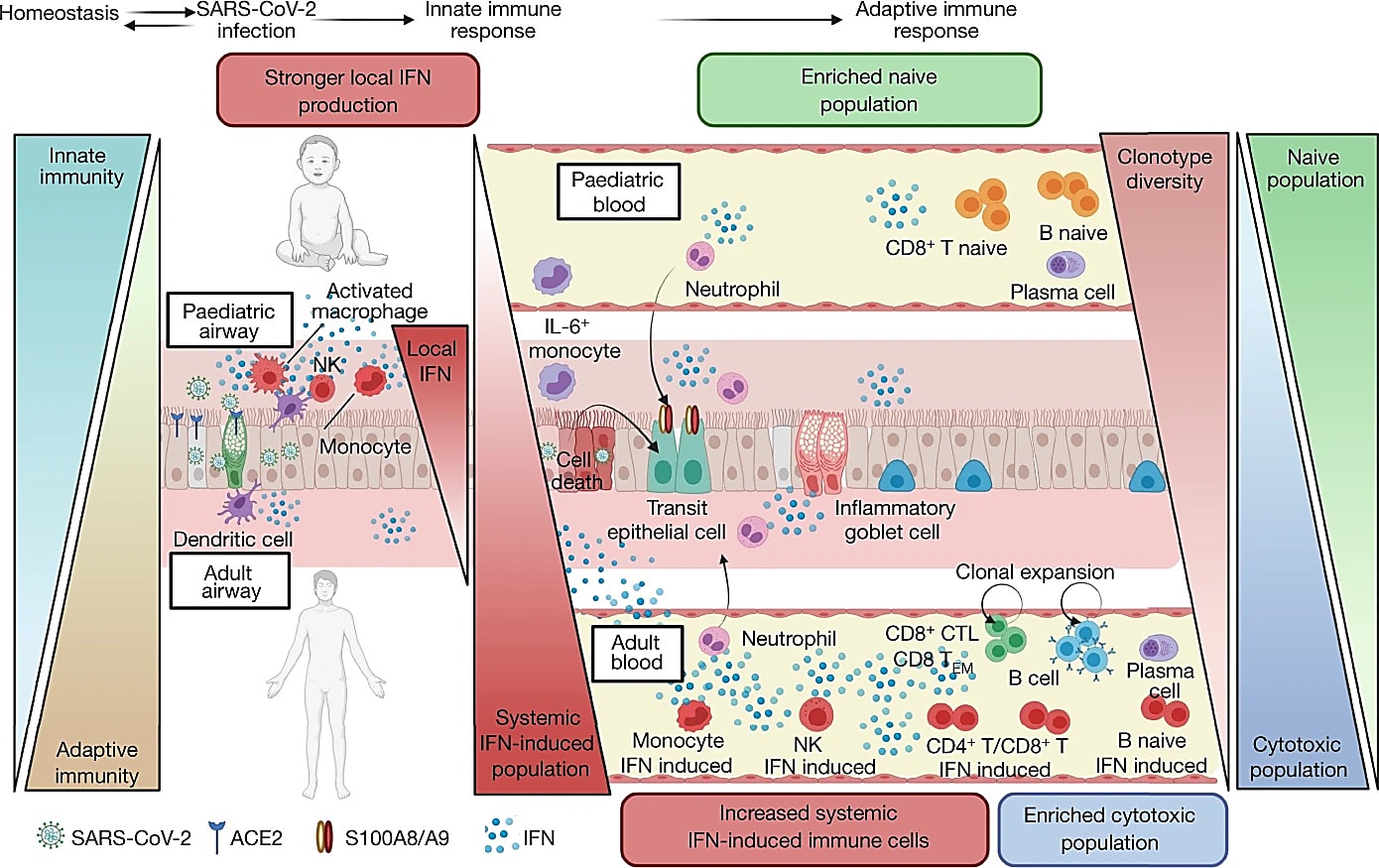
As this study demonstrates, it turns out that we can learn a lot about fighting infectious diseases from our children. The preactivated airway epithelium in children may function to restrict the spreading of viruses. At the same time, the naive state of the immune system in the blood presents a broader pool of immune receptors available to detect new pathogens. With these insights into how the immune system responds during childhood and into adulthood, researchers and physicians have new avenues to explore as they seek to better understand patient outcomes.
References:
- Hu, JC. (2019, May 1). A brief history of cooties. Smithsonian.com. Retrieved February 4, 2022, from https://www.smithsonianmag.com/history/brief-history-cooties-180971914/
- American Academy of Pediatrics and the Children’s Hospital Association. Children and COVID-19: State-level data report. American Academy of Pediatrics. Retrieved February 7, 2022, from https://www.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-state-level-data-report/
- Castagnoli R, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review. JAMA Pediatr 174: 882–889 (2020).
- World Health Organization. Child mortality (under 5 years). World Health Organization. Retrieved February 8, 2022, from https://www.who.int/news-room/fact-sheets/detail/levels-and-trends-in-child-under-5-mortality-in-2020
- Yoshida M, et al. Local and systemic responses to SARS-CoV-2 infection in children and adults. Nature 602: 321–327 (2022). https://doi.org/10.1038/s41586-021-04345-x
